Lifeline Amid Ethical Challenges
ORGAN TRANSPLANTATION IN INDIA
A Lifeline Amid Ethical Challenges
Rishikesh Kumar*
“When life takes a tragic turn, it can still offer hope,” said the father of Vaidehi Bhau Tanavde, a 12-year-old girl who was declared brain-dead following a rare auto-immune illness. In the face of unimaginable loss, her family made the courageous decision to donate her organs, giving four people in Mumbai a second chance at life.
Vaidehi’s story is one of rare courage and compassion in a country where organ donation rates remain alarmingly low. Despite a population of over 1.4 billion, the number of organ donors annually falls short of the demand by a staggering margin. Over 500,000 people require organ transplants each year, but less than 15,000 donations take place.
Organ donation is a powerful way to save lives, but in India many people are unsure about how it works or what it takes to become a donor. In this article, we’ll explore the basics of organ donation in India—how it works, who can donate, and what the process looks like for everyday people.
We’ll also look at some important questions: Are organ donations fair and equal? How do money, cultural beliefs, or religion affect people’s decisions to donate?
We will examine these questions through ethical lenses, providing a deeper understanding of the challenges and opportunities in organ donation and why it’s a cause worth engaging with and supporting.
Understanding Organ Donation
The process of organ transplantation involves the surgical removal of a healthy organ from a donor and its transplantation into the body of a recipient suffering from organ failure. For many, this procedure is a life-saving intervention, offering a second chance at life when all other medical options have been exhausted. Without such transplants, patients with end-stage organ failure often face a bleak prognosis.
Organ donation in India is governed by the Transplantation of Human Organs and Tissues Act of 1994, which ensures that anyone, regardless of age, caste, religion, or community, can choose to donate their organs
Tissue donation, while less publicised, is equally impactful. It can significantly improve the quality of life for recipients, restoring vital functions and offering a path to recovery
Organ donation, at its core, is an altruistic act. For an individual, it involves pledging during their lifetime that their organs can be used after their death to save lives. This selfless decision has the potential to transform despair into hope, allowing patients with failing organs to lead healthy, productive lives.
By bridging the gap between a healthy donor and a patient in need, organ transplantation underscores the profound impact of human kindness and medical science. It is a powerful way to leave a lasting legacy—offering life, even in death.
Eligibility in India
Organ donation in India is governed by the Transplantation of Human Organs and Tissues Act of 1994, which ensures that anyone, regardless of age, caste, religion, or community, can choose to donate their organs. While people above 18 years are generally preferred, the key factor for eligibility is the donor’s overall health, not just their age.
Medical Ethics and Bioethics
Medical ethics is the set of moral principles that guide the practice of medicine. It ensures that doctors and other healthcare professionals provide fair, respectful and principled care, regardless of a person’s gender, religion or race. Key principles of medical ethics include respect for autonomy (allowing patients to make informed decisions about their care), justice (fair treatment and equal access to resources), and compassion (acting in the patient’s best interest). In organ donation, medical ethics plays a crucial role in ensuring fairness in the allocation of scarce resources like organs, while also respecting the donor’s and recipient’s choices and dignity
Bioethics, on the other hand, is a broader field that examines moral principles in all areas of life sciences, including medicine, biotechnology, politics and law. It goes beyond the clinical focus of medical ethics and includes the societal, cultural and philosophical dimensions of healthcare. For example, bioethics helps us consider how cultural beliefs, socioeconomic conditions and even advancements in science affect organ donation decisions.
While medical ethics provides a framework for fair and patient-centred care, bioethics encourages us to address the larger systemic and societal
While medical ethics provides a framework for fair and patientcentred care, bioethics encourages us to address the larger systemic and societal barriers to organ donation.
barriers to organ donation. Both perspectives are essential to understanding and improving the process. Whether you choose to view organ donation through the precise lens of medical ethics or the broader approach of bioethics, the goal remains the same—to create a system that respects human dignity and fosters equitable access to lifesaving care.
Types of Organ Donation
Living Organ Donation: Living organ donation is a remarkable medical practice where a healthy organ is transplanted from a living donor to a patient suffering from end-stage organ failure. This form of donation is most commonly seen in cases of kidney or liver failure, where timely transplantation can mean the difference between life and death.
For example, in liver donation, a portion of the donor’s liver is surgically removed and transplanted into the recipient. What makes this unique is the liver’s ability to regenerate itself, allowing both the donor’s and recipient’s livers to grow back to their normal size over time. Similarly, kidney donation involves the removal of one kidney, enabling the donor to continue leading a healthy and active life with the remaining kidney.
Living donors are typically close family members, such as parents, siblings, or children, though they can also be distant relatives or close friends. The selflessness of living donors highlights the profound human capacity for generosity and compassion, offering a lifeline to patients whose organs have failed.
There are three main types of living organ donation:
Directed Donation: The donor chooses the recipient, often a close family member such as a spouse, parent, child, sibling, or grandparent. This is the most common type of living donation.
Non-Directed Donation: The donor has no personal connection to the recipient and donates purely for altruistic reasons. The recipient is selected based on medical compatibility.
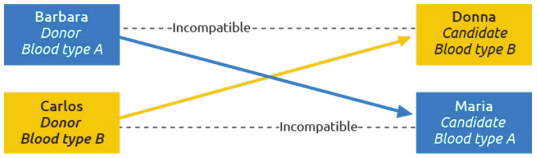
Paired Donation (Kidney Swap): This involves two donor-recipient pairs who exchange kidneys when the original donor-recipient match is incompatible. This innovative approach ensures both recipients receive compatible kidneys.
Living donors are eligible to donate the following organs:
- One of their kidneys
- A portion of the pancreas
- Part of the liver.
Deceased Donors: A deceased donor has the potential to save multiple lives by donating six essential organs: kidneys, liver, heart, lungs, pancreas, and intestine. While organs like the uterus can also be transplanted, they are not considered lifesaving. Organ donation can only proceed after the donor is declared legally dead and the family provides their consent.
In India, brainstem death is legally recognised as a form of death, enabling the donation of vital organs. In such cases, up to 37 organs and tissues, including the six life-saving organs, can be donated. After natural cardiac death, tissues such as corneas, bones, skin, and blood vessels can also be donated, offering hope and healing to many.
How to be a Donor
By filling out an online pledge form through Organ India, you can take the first step toward saving lives and receive a donor card, complete with a unique government registration number from the National Organ and Tissue Transplant Organisation. Here’s how you can get started in just a few easy steps:
Online Pledge Form: To start, visit the Organ India website at https://bit.ly/4eTBDxr
Fill out the online pledge form, which allows you to officially declare your intent to donate your organs. After completing the form, you’ll receive a donor card with a unique government registration number from the National Organ and Tissue Transplant Organisation (NOTTO).
Once you’ve registered, your pledge is automatically recorded with NOTTO, the national body responsible for organ donation. This ensures that your decision to donate is officially recognised and can be referred to when needed.
While registering is a crucial step, it’s equally important to talk to your family about your decision to donate your organs. In India, even if you have pledged to donate, the consent of your next of kin is necessary after your passing. Having this conversation ensures your family is aware of and supports your wishes.
Ethics, Biology and Human Values
A number of questions encourages us to think deeply about the connection between ethics, biology, and human values.
Is healthcare merely a profitdriven business model, or should it prioritise the essential medical services needed by patients?
Should healthcare operate purely as a professional service, devoid of any moral responsibility or focus on patient welfare?
Does an individual in need of an organ to survive have a moral right to claim the organ of another person?
Is it legally justifiable to treat human organs as commodities, selling them to wealthy individuals instead of prioritising the poor and needy? Isn’t the life of a poor person just as valuable as that of a wealthy one?
How should healthcare resources like human organs, which are necessarily limited, be made available?
As members of society, what responsibilities do healthcare professionals have toward the common good and public interest?
By looking at these questions through a bioethical lens, we can find perspectives that help shape fair policies, responsible practices and thoughtful individual decisions, all while respecting the dignity of everyone involved.
Organ transplantation is a lifesaving medical advancement that demands a careful balance of moral, social and legal considerations. At its core is the principle that human beings are not commodities; decisions about organ donation and transplantation must respect human dignity and equity.
Equity and Access
A key concern is whether organ transplantation ensures fair access for all, regardless of socio-economic status. The reality often favours the wealthy, as transplantation is costly and policies may prioritise those with better resources. Vulnerable groups, such as women, minorities, the elderly, and the disabled, remain under-represented in receiving transplants, highlighting systemic inequities.
The phenomenon of ’transplant tourism’ exacerbates disparities, where patients from wealthier nations procure organs from poorer regions, sometimes through unethical means, including trafficking and coercion. Such practices call for stringent enforcement of laws to protect vulnerable populations.
Culture and Religion
Cultural and religious beliefs significantly shape attitudes toward organ donation. While some religions view donation as a noble act, others resist due to differing views on brain death or the sanctity of the body. These beliefs influence both individual decisions and national transplant policies, requiring sensitive engagement and education.
Trust and Consent
Trust is essential in organ transplantation but is often strained in large, impersonal healthcare systems. Some patients fear carrying donor cards, suspecting it might compromise their care. Informed consent, rooted in clear and compassionate communication, is critical to rebuilding trust and ensuring ethical practices.
Distributive Justice
The principle of distributive justice demands fairness in organ allocation, but no universal standard exists. Should priority be given to those most likely to survive, those most socially valuable, or through random
A key concern is whether organ transplantation ensures fair access for all, regardless of socio-economic status. The reality often favours the wealthy, as transplantation is costly and policies may prioritise those with better resources.
allocation? Balancing these criteria remains a challenge.
A Human Approach
Organ transplantation must prioritise equity, ensuring that rich and poor, men and women, and diverse cultural groups are treated fairly. Legal and ethical systems must safeguard human dignity, combat organ trafficking and foster trust. Only by addressing disparities and respecting cultural diversity can transplantation truly reflect justice and compassion.
“To the world, you might be one person, but to one person, you might be the world.” These words remind us how powerful a single act of kindness can be. By pledging to become an organ donor, you have the chance to save lives and give someone a future they thought they’d lost. Every day, thousands of people wait for organ transplants, clinging to hope. You could be the reason their story continues.
Charting New Paths
Organ donation is no longer just about saving lives—it’s also about improving the quality of life through groundbreaking transplants like those of the face, hands, uterus, etc. This quiet revolution calls for a fresh perspective on the ethical questions surrounding organ donation. As technology advances and we achieve state-of-the-art medical breakthroughs, it’s important to ask, are we ensuring humanity, equality, compassion, freedom of choice, and a level playing field for everyone?
In a diverse country like India, where cultural, religious, and socioeconomic factors play a significant role, these questions become even more critical. Organ donation has the power to transform lives, but for it to truly benefit society, it must be guided by principles that respect every individual and promote fairness and dignity for all. It’s up to each of us to understand these issues, make informed decisions, and support a system that balances innovation with ethical responsibility.
NEXT »



